When the Department of Health and Social Care published Fit for the Future last summer, it did more than set out another set of targets. The plan is an open invitation to rethink care itself: to move treatment out of hospitals and into neighbourhoods; to replace paper and pagers with data flows; and to stop reacting to sickness only after it takes hold. At the centre of every pledge is the same expectation—that digital, AI-powered tools will do much of the heavy lifting.
Yet technology on its own delivers nothing. What matters is how people and organisations bring it to life. StabiliseAI was founded for precisely that practical gap: to curate real-world evidence, demystify the marketplace and make sure every trust, ICB and supplier can move at pace without losing sight of patients or budgets.
From policy to practice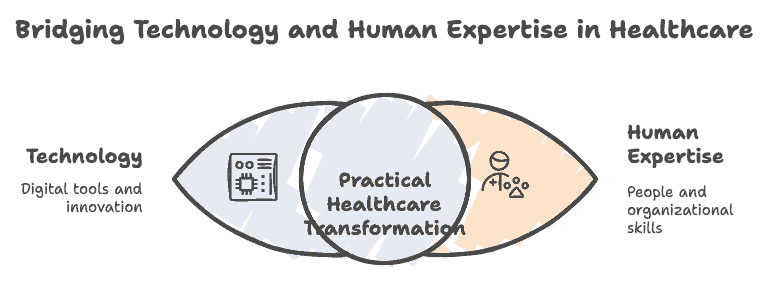
The Plan’s first promise is a “doctor in your pocket” NHS App. By 2028 it should book tests, surface records and let citizens manage long-term conditions without endless phone queues. Simple in principle, revolutionary in effect. Every digital front door that works smoothly removes friction from clinical time, cuts did-not-attend rates and, crucially, makes services more equal—because the poorest communities are the ones who lose most time travelling or waiting.
Behind that screen sits a second pledge: AI scribes and decision support at scale. Automatic transcription is no gimmick; early pilots show that freeing just ninety seconds from each consultation returns the equivalent of two thousand full-time GPs across England. Multiply that saving across nursing handovers, radiology reporting or pharmacy reconciliation and the productivity dividend begins to dwarf incremental funding rounds.
Our line-chart above projects what that roll-out might look like if the NHS really does become “the most AI-enabled care system in the world”. A ten-percentage-point jump in AI-ready pathways every two years may feel ambitious, but it mirrors what happened when digital imaging replaced film a decade ago: once early adopters prove safety and worth, uptake accelerates.
Building a neighbourhood health service
Technology matters even more outside hospital walls. The Plan talks of shifting spend—and therefore staff—into new Neighbourhood Health Centres, backed by a single, longitudinal patient record. That record, enriched with genomic risk scores or wearable feeds, allows care to pivot from patch-up to prevention. Community nurses can see which frailty patients are trending towards a fall; mental-health teams can intervene before a crisis tips someone into A&E.
For commissioners and digital leads the challenge is choosing the right building blocks. In the interactive table you’ll find four flagship initiatives matched with the digital enablers they depend on—plus the specific ways Stabilise AI already supports them, from ROI calculators for AI scribes to governance templates for population-health dashboards.
Money, motivation and trust
None of this is cheap, but it is less costly than the alternative. Two-thirds of current outpatient appointments, worth about £14 billion a year, are earmarked for replacement by remote advice or patient-initiated follow-up. Hospital-at-home pathways, underpinned by automation and remote monitoring, cost around a fifth of an inpatient bed. The Plan also introduces a new choice charter that will publish real-time outcome data on the App. Choice backed by transparency creates a virtuous loop: providers that embrace innovation win loyalty, while laggards feel patient and financial pressure to improve.
That same transparency must extend to algorithms themselves. Patients will only trust an AI triage bot—or a genomic risk alert—if they know who is accountable when something goes wrong. Stabilise AI therefore places as much weight on ethics, explainability and inclusive design as on coding prowess. Human-centred technology should never widen the digital divide; it should shrink it.
Where Stabilise AI adds value
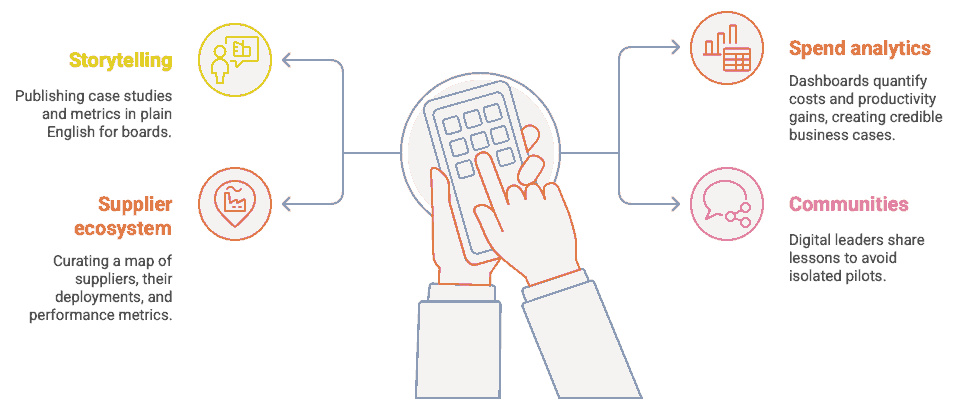
-
Storytelling with evidence. We publish case studies and metrics in plain English, so boards can compare options without spin.
-
Spend analytics. Our dashboards quantify whole-life costs and productivity gains, turning “nice idea” into credible business case.
-
Supplier ecosystem. From start-ups to blue-chips, we curate a living map of who does what, where they are deployed and how they perform.
-
Communities of practice. Digital chiefs, clinicians and patient advocates share lessons early—avoiding siloed pilots that never scale.
Looking ahead
The next twelve months will decide whether the Ten-Year Plan gains momentum or stalls in worthy rhetoric. Success depends on three things: a workforce that feels ownership of AI tools rather than fear; data standards that let innovators plug-and-play safely; and a shared narrative that keeps the spotlight on better outcomes, not shinier apps.
Stabilise AI will be tracking that progress every step of the way—celebrating wins, challenging hype and, above all, ensuring that digital transformation remains a means to an end: smarter care, empowered patients, and an NHS that is both equitable and sustainable for generations to come.